Tonsil Stone Question From Reader
Message: Hello Dr. Zhou,
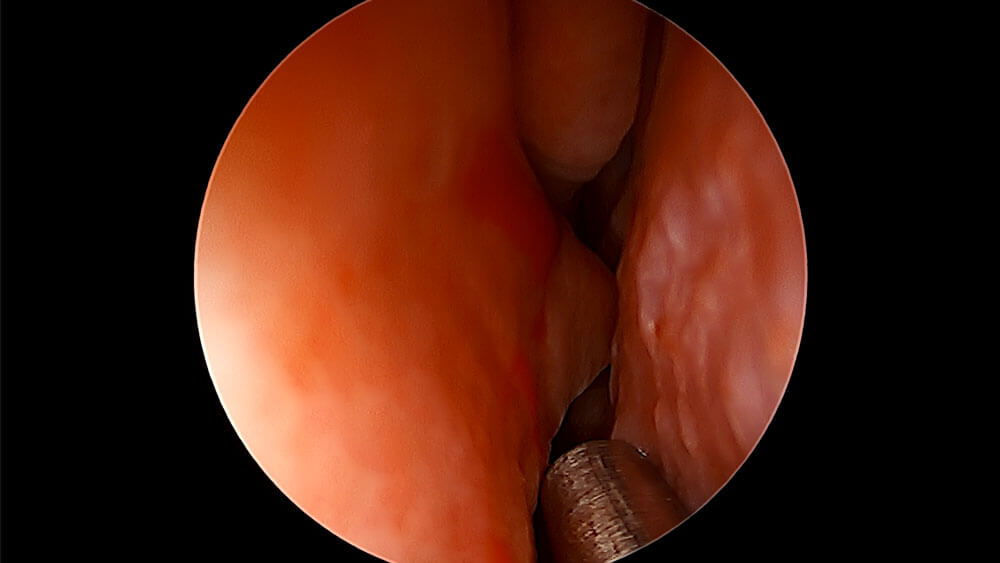
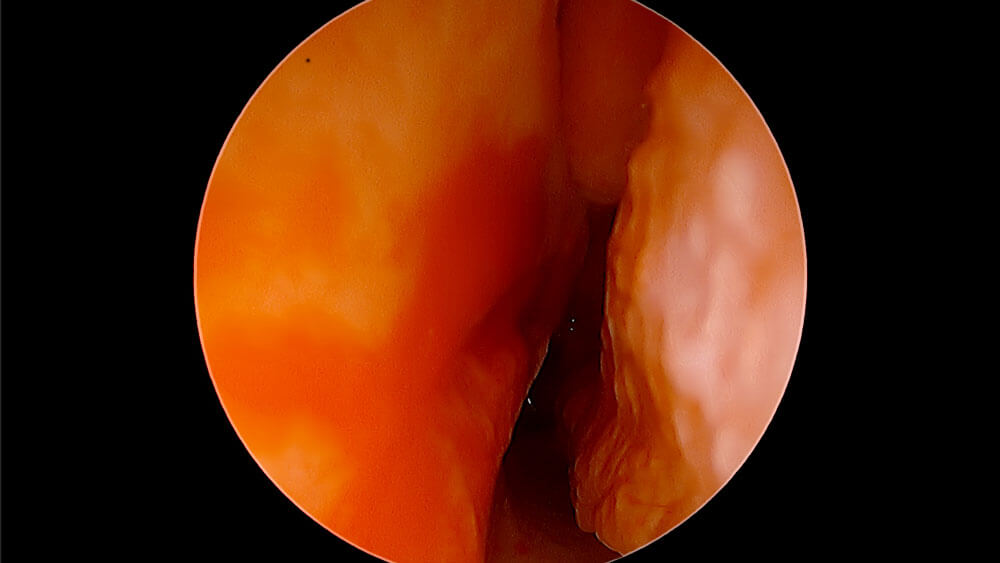
I have a question about tonsillectomies. I just read your blog post and listened to the episode on tonsils. I recently went to my family doctor and he recommended getting my tonsils removed because he said they are large and have redness, holes, and white spots. I have not followed up with an ENT yet (I am living in NC currently). I continue to get tonsil stones and have removed some of them with QTips. I have noticed the tonsil stones continuing to appear for about 6 months now. I have had about 4 cases of severe sore throat throughout the past year, but the strep tests came back negative all but one time. Here lately my throat just feels raw and my glands are swollen. I am nervous about surgery as I know it is worse for adults. I also react poorly to pain medication and have vomited after every surgery I have ever had and ended up back in the ER due to this. I know that would be very painful after a tonsillectomy. I really just want to not deal with the sore throat but also don’t want to get my tonsils taken out. I know it’s hard to say without looking at my tonsils, but what would you recommend? Is there anything I can do to prevent the tonsil stones from returning or to get rid of them? Thank you so much for your time!
My Reply: